Introduction
Nose fillers have become an increasingly popular non-surgical alternative to traditional rhinoplasty, offering patients a quick and minimally invasive way to reshape their noses. However, as with any cosmetic procedure, there’s always some potential risks you should be aware of. One such risk centres around the question, ‘Does nose filler migrate?‘.
While relatively rare, nose filler migration can lead to undesirable aesthetic outcomes and, in even rarer cases if unmanaged, medical complications such as blocking a blood vessel. As the demand for surgical and non-surgical rhinoplasty continues to grow, with an estimated 67% increase in procedures in 2022 compared to the previous year according to the British Association of Aesthetic Plastic Surgeons (BAAPS), it’s more important than ever for potential patients to be well-informed about all aspects of the treatment, including the possibility of filler migration.
When nose filler goes well, it can be transformative, as demonstrated in one of my clients below.

But when it migrates, which although very rare and prevented in my clinic, it can start to overshadow the results.
In this post, we’ll explore nose filler migration, its signs and symptoms, and the underlying causes. By going into these topics, we aim to provide you with the knowledge necessary to make informed decisions about your aesthetic journey. Whether you’re considering nose fillers for the first time or have already undergone the procedure, understanding the potential for migration should be an important part of your decision-making process.
What is Nose Filler Migration?
Nose filler migration refers to the movement of dermal filler material from its intended injection site to another area within the facial region. This displacement can occur immediately after the procedure or develop gradually over time. While hyaluronic acid-based fillers are designed to integrate with the surrounding tissue, various factors can cause them to shift, leading to unintended changes in the nose’s appearance or affecting nearby facial structures.
It’s important to note that filler migration is not unique to nose procedures; it can occur with dermal fillers used in any part of the face. However, the nose’s complex anatomy and its central position on the face make migration in this area particularly noticeable and concerning. Studies have shown that while the overall incidence of filler migration is low, estimated at around 1-3% of all dermal filler procedures, the risk may be slightly higher in nasal treatments due to the area’s unique characteristics and the technical challenges involved in precise placement. To put this into perspective, a 5-year review of filler complications found that the overall incidence of complications from dermal fillers was only 0.7% (14 out of 2,089 procedures), with HA dermal filler (the type typically used in non-surgical rhinoplasty) only making up 2 of those 14 complications. As procedures go, this is an extremely low complication rate, which is positive all round.
Signs and Symptoms of Nose Filler Migration
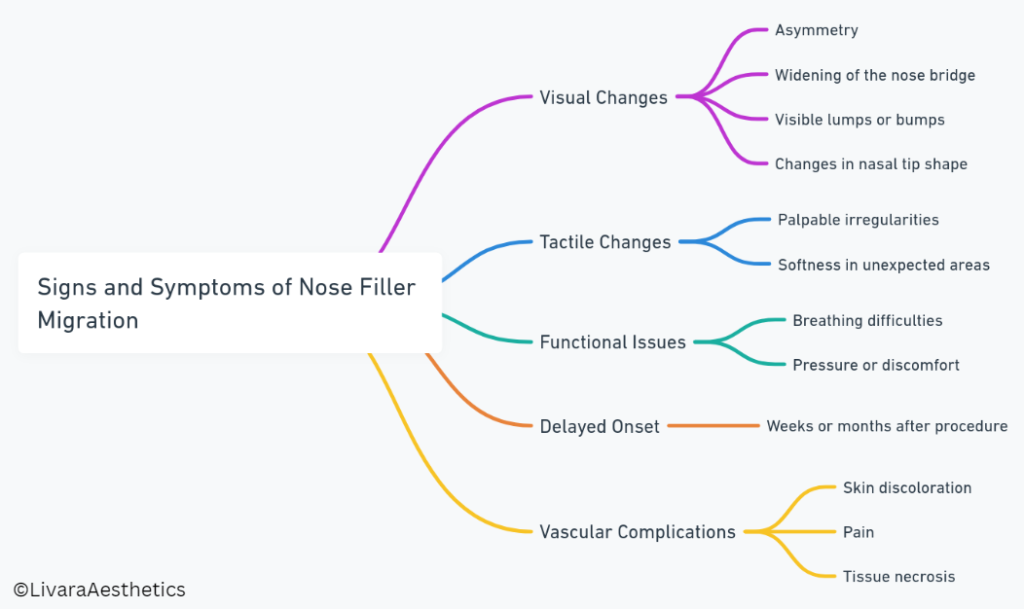
Recognising the signs and symptoms of nose filler migration, such as redness or a bruise, is vital for early intervention and optimal management. While some changes may be subtle, others can be quite noticeable, affecting both the aesthetic outcome and, in rare cases, the functional aspects of the nose. Here are the key indicators to watch for:
- Visual Changes:
- Asymmetry: One side of the nose may appear fuller or more elevated than the other.
- Widening of the nose bridge: This can create an unnatural, overfilled appearance.
- Visible lumps or bumps: These may appear in areas where filler was not initially injected.
- Changes in nasal tip shape: The tip may become bulbous or appear to droop.
- Redness or bruising: An area may begin to show discolouration if the migration starts to restrict blood flow.
- Tactile Changes:
- Palpable irregularities: You may feel small, movable lumps under the skin.
- Softness in unexpected areas: Parts of the nose may feel unusually soft or squishy.
- Functional Issues:
- Breathing difficulties: In rare cases, significant migration can affect nasal passages.
- Pressure or discomfort: Some patients report a sensation of fullness or pressure.
- Delayed Onset:
- It’s important to note that signs of migration may not appear immediately. Some patients report changes weeks or even months after the initial procedure.
- Vascular Complications:
- While extremely rare, severe cases of migration can lead to vascular occlusion, presenting as skin discoloration, pain, or in the most serious instances, tissue necrosis.
According to a 2022 study published in the Aesthetic Surgery Journal, approximately 85% of filler migration cases are identified within the first six months post-procedure. However, the remaining 15% may present later, emphasising the need for ongoing awareness and follow-up.
If you notice any of these signs or symptoms, it’s crucial to consult with your practitioner promptly. Early detection and intervention can often mitigate the effects of migration and prevent more serious complications from developing.
Causes of Non-Surgical Nose Filler Migration
Understanding the causes of nose filler migration is essential for both practitioners and patients in minimising risks and achieving optimal, long-lasting results. While the exact mechanisms of migration are still being studied, several key factors have been identified:
- Injection Technique:
- Overfilling: Excessive amounts of injectable filler can create pressure, forcing the material to spread.
- Improper Depth: Placing filler too superficially or too deeply can lead to unintended movement.
- High-Pressure Injection: Rapid or forceful derma filler injections can disperse filler beyond the target area.
- Filler Properties:
- Viscosity and Cohesivity: Less viscous or cohesive fillers are more prone to migration.
- Hydrophilic Nature: Some fillers attract water, potentially leading to expansion and movement.
- Anatomical Factors:
- Facial Muscle Activity: Regular movements of facial muscles can gradually displace filler.
- Vascular Anatomy: The nose’s complex blood supply can influence filler distribution.
- Patient Behavior:
- Excessive Touching or Massaging: Manipulating the treated area post-procedure can shift filler.
- Sleeping Position: Consistent pressure from certain sleeping positions may affect filler placement.
- Time and Gravity:
- Natural Aging Process: As skin loses elasticity over time, filler may shift.
- Gravitational Pull: Especially relevant for heavier or less cohesive fillers.
- Immune Response:
- Foreign Body Reaction: In some cases, the body’s immune response can alter filler distribution.
- Practitioner Experience:
- Lack of Expertise: Inexperienced injectors may not fully account for the nose’s unique anatomy.
A study published in the Plastic and Reconstructive Surgery Journal in 2021 found that approximately 60% of migration cases were primarily attributed to injection technique, while 25% were linked to filler properties, and the remaining 15% were due to a combination of patient factors and anatomical considerations.
It’s important to note that while these factors can contribute to migration, the risk is significantly reduced when treatments are performed by experienced, medical professionals using high-quality products. Patients can also play a role in prevention by following post-procedure care instructions diligently during their recovery time and choosing reputable clinics for their treatments.
How I Minimise Risk of Filler Migration in my Clinic
In my clinic, preventing filler migration is a top priority, and I’ve developed a comprehensive approach to minimise this risk. My strategy begins well before the actual treatment and continues through the aftercare phase.
First, patient selection and education are necessary. During the initial consultation, I thoroughly assess each patient’s facial anatomy, skin quality, and previous treatment history to ensure the safest approach to their injectable treatment. I take the time to explain the procedure, including potential risks like migration, and set realistic expectations. This open dialogue during the treatment plan helps patients understand the importance of following aftercare instructions and reporting any concerns promptly.
When it comes to product selection, I exclusively use high-quality hyaluronic acid fillers with appropriate rheological properties for nasal augmentation. These fillers have a higher G’ (elastic modulus) and cohesivity, which helps them maintain their shape and position after injection. HA fillers with higher viscosity and cohesivity are generally preferred for nose augmentation, as they tend to stay in place better than softer, more fluid formulations. These firmer fillers provide the structural support needed for nose reshaping while resisting displacement due to natural facial movements.

I always prefer the ‘less is more’ approach when it comes to aesthetics, but especially for non-surgical rhinoplasty (also known as a liquid nose job). This is because overfilling is a common cause of migration, so as an experienced practitioner I mitigate against this by using smaller amounts of filler, often over multiple sessions, to achieve the desired result. This gradual approach allows me to assess the outcome at each stage and make subtle adjustments, reducing the risk of overcorrection and subsequent migration.
My injection technique is meticulous and tailored to each patient’s unique nasal anatomy. I inject on the bone as it greatly reduces the risk of intravascular injection. I always inject slowly and with minimal pressure, using small aliquots of filler to achieve the desired result gradually and reduce the risk of product displacement. This approach not only reduces the risk of migration but also allows for more natural-looking outcomes.
Post-treatment, I provide detailed aftercare instructions to my patients, both verbally and in writing. These include:
- Avoiding touching or massaging the treated area for at least 48 hours
- Refraining from wearing glasses or sunglasses for 3-5 days
- Sleeping with the head elevated for the first few nights
- Avoiding strenuous exercise for 24-48 hours
I also schedule a follow-up appointment within two weeks of the procedure to assess the results and address any concerns. This proactive approach allows for early detection and management of any potential complications, including migration.
By combining these strategies – careful patient selection, appropriate product choice, refined injection technique, and comprehensive aftercare – I’ve been able to significantly reduce the incidence of filler migration in my clinic, ensuring safer and more satisfactory outcomes for my patients.
What to Do if You Suspect Filler Migration
If you suspect filler migration in your nose or any other treated area, it’s crucial to act promptly and seek professional advice. The first step is to contact the practitioner who performed your treatment. They are familiar with your medical history and the specific product and technique used, making them best equipped to assess your situation.
During your follow-up appointment, your practitioner will conduct a thorough examination. This typically involves visual inspection and gentle palpation of the treated area to detect any irregularities or displacement of the filler. They may also review before and after photos to compare the current appearance with the immediate post-treatment results.
If filler migration is confirmed, the course of action will depend on several factors, including the extent of migration, the type of filler used, and the time elapsed since the treatment. For hyaluronic acid-based fillers, which are most commonly used in liquid rhinoplasty, the primary treatment option is dissolution using hyaluronidase.
Hyaluronidase is an enzyme that breaks down hyaluronic acid, effectively reversing the effects of the filler. The procedure involves injecting small amounts of hyaluronidase into the affected area, which under normal activity can dissolve the migrated filler within 24-48 hours, avoiding the complications of a non-surgical nose filler gone wrong. It’s important to note that while hyaluronidase is highly effective, it may also dissolve some of the correctly placed filler, potentially necessitating a touch-up treatment later.
In cases where migration is minimal and not causing significant aesthetic or functional issues, your practitioner might recommend a ‘watch and wait’ approach. Hyaluronic acid fillers naturally break down over time, so minor migration may resolve on its own without intervention.
For non-hyaluronic acid fillers, management can be more challenging as there is no specific dissolving agent. In these cases, treatment options may include steroid injections to reduce inflammation, massage techniques to redistribute the filler, or in rare cases, surgical removal.
Remember, early detection and professional intervention are key to managing filler migration effectively. Regular follow-up appointments and open communication with your practitioner can help ensure any issues are addressed promptly, maintaining both the safety and aesthetic quality of your non-surgical rhinoplasty results.
Conclusion
Non-surgical rhinoplasty using dermal fillers has revolutionised the field of aesthetic medicine, offering patients a quick, minimally invasive option for nose reshaping. However, as with any medical procedure, it comes with potential risks, including filler migration. Understanding these risks, their causes, and how to prevent and manage them is crucial for both practitioners and patients.
While migration is a possibility, it’s relatively rare when the procedure is performed by experienced, qualified practitioners using appropriate techniques and high-quality products.
If you’re considering non-surgical rhinoplasty, hopefully, this information will empower you to make an informed decision and ask the right questions when selecting a practitioner.
Remember, while the possibility of complications exists, the vast majority of patients enjoy successful, satisfying results from their non-surgical nose jobs. With proper precautions and expert care, nose filler treatments remain a safe and effective option for those seeking to enhance their facial aesthetics without surgery, avoiding the need for surgical nose alterations.